Abstract
The application of multiphoton microscopy in the field of biomedical research and advanced diagnostics promises unique insights into the pathophysiology of inflammatory skin diseases. In the present study, we combined multiphoton-based intravital tomography (MPT) and fluorescence lifetime imaging (MPT-FLIM) within the scope of a clinical trial of atopic dermatitis with the aim of providing personalised data on the aetiopathology of inflammation in a non-invasive manner at patients’ bedsides. These ‘optical biopsies’ generated via MPT were morphologically analysed and aligned with classical skin histology. Because of its subcellular resolution, MPT provided evidence of a redistribution of mitochondria in keratinocytes, indicating an altered cellular metabolism. Two independent morphometric algorithms reliably showed an even distribution in healthy skin and a perinuclear accumulation in inflamed skin. Moreover, using MPT-FLIM, detection of the onset and progression of inflammatory processes could be achieved. In conclusion, the change in the distribution of mitochondria upon inflammation and the verification of an altered cellular metabolism facilitate a better understanding of inflammatory skin diseases and may permit early diagnosis and therapy.
Introduction
Atopic dermatitis (AD) is a highly prevalent inflammatory skin disease with increasing incidence, mainly in developed countries. Manifestation of AD usually occurs in early childhood and is often followed by the development of allergies and asthma. According to current data, approximately 10–30% of newborns are affected by AD1. The underlying pathophysiological mechanisms of the disease are under debate, and a complex interplay between genetic, epigenetic and environmental factors is suggested2. However, further knowledge of the pathophysiology of AD is essential to improve the present therapeutic options.
To overcome the limitations of current mouse models and the restricted ability to analyse the skin of human patients via invasive techniques such as biopsies, we have applied multiphoton-based intravital tomography (MPT) equipped with a spectral fluorescence lifetime imaging module3 (MPT-FLIM) for the non-invasive in vivo analysis of human skin. Currently, the diagnosis of skin diseases is mainly based on the skills of the dermatologist or on the histological analysis of biopsies (the current gold standard). Physical examination of the patient is limited to the macroscopic surface level, and taking biopsies is an invasive approach, resulting in the formation of scars, thus excluding a longitudinal analysis of specific skin lesions. In contrast to alternative in vivo techniques such as ultrasound or confocal laser scanning microscopy4, MPT-FLIM allows subcellular in vivo imaging of thus far unknown parameters of inflammation. Therefore, the aim of the present study was to validate multiphoton-based tomography as a unique non-invasive tool for the morphological and biochemical characterisation of human skin.
Five-dimensional MPT-FLIM analysis comprises spatial (first to third dimension) and spectrally resolved fluorescence lifetime imaging (fourth and fifth dimension) by means of femtosecond laser pulses. This laser technology allows deep penetration of light into the skin and therefore the visualisation of the epidermis as well as the upper part of the dermis with subcellular resolution. In vivo investigations in humans exclude the application of fluorescence labelling of cells or proteins but are open to the use of naturally occurring fluorophores, such as melanin, keratin or NADH5,6. Multiphoton excitation of these endogenous fluorophores therefore enables the non-invasive high-resolution examination of human skin without damaging the surrounding tissue7.
Previous in vitro studies applying multiphoton microscopy showed a link between the pro-inflammatory activation of macrophages and the NADH signal intensity, suggesting an increased production of reactive oxygen species and a rearrangement of cellular metabolism8. To determine the cellular metabolism of epidermal cells in vivo, we utilised MPT-FLIM, an approach that enables an excitation energy independent readout of the NADH status9,10. In vivo FLIM measurement of NADH has been used in the context of skin cancer diagnoses in rodents11 and was recently successfully applied in the clinic12,13,14. The FLIM signal depends strongly on the microenvironment of the excited substance, enabling the discrimination of protein-bound and free NADH15. Free NADH was found to exhibit a fluorescence lifetime between 200 and 450 ps, whereas protein-bound NADH exhibits a prolonged lifetime in the range of 2,000 to 3,000 ps16,17. The ratio of free to protein-bound NADH is reflected by the mean fluorescence lifetime (taum)18, which serves as an intravital readout of the cellular metabolic state19.
Our clinical trial comprised 45 patients and followed their individual inflammatory progression over three months. For the first time, we established MPT-FLIM as a reliable and valuable tool for the clinical investigation of inflammatory skin diseases, facilitating a rapid, cost-efficient, non-invasive in vivo examination for diagnostic and therapeutic purposes in humans.
Results
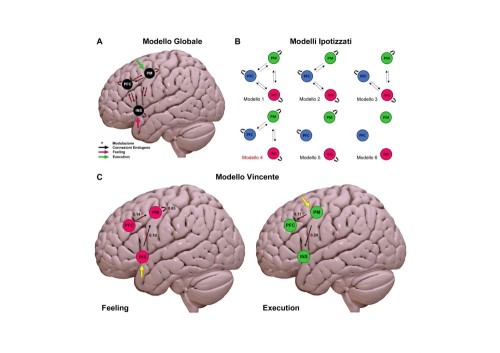
Alignment of intravital multiphoton tomographic data with classical skin biopsy analysis
We used MPT as an artefact-free, painless approach that provides an ‘optical biopsy’ with subcellular resolution in human skin (Fig. 1a, see also Supplementary Movie S3). Previous studies of multiphoton imaging have suggested that NADH is the major natural fluorophore in human cells20,21,22. The bright spots observed in the cytoplasm of keratinocytes surrounding dark nuclei when using this technique (Fig. 1b) are mainly due to multiphoton-excited NADH, ensured by the combination of the utilised excitation wavelength and spectral emission filtering (see Methods section). These spots are located within the mitochondria as shown by immunohistochemical and fluorescence microscopic alignment (Fig. 1). Based on these settings, we compared the same skin region in healthy subjects and patients affected by AD via MPT and subsequently via histological analyses (Fig. 2). It must be emphasised that MPT allows horizontal sectioning of the skin, and we therefore also collected comparative biopsies cut in a horizontal manner. Each subject was clinically examined by a dermatologist and by MPT over a period of three months. During each session, we analysed one lesional (inflamed tissue) and one non-lesional (ostensibly healthy) skin region in comparison to the areas in age-correlated healthy subjects. As shown in Fig. 2, the analyses of histological biopsies and multiphoton-based intravital tomographic images of lesional skin areas were of identical pathognomonic validity (compare ‘hist.’-columns and skin depth correlated ‘MPT’-columns, Fig. 2b–e). Upon MPT, we were able to detect the characteristic skin morphologies of AD, such as intercellular oedema and an impaired architecture, accompanied by thickening of the epidermis in lesional skin. In particular, due to the absence of artefact-inducing embedding, dehydration and staining procedures, the MPT technique is markedly superior regarding assessment of the intensity of intercellular oedema (Fig. 2d, AD lesional, marked with a blue box).
Ultimi Articoli
Lombardia: prima legge regionale sull’Intelligenza Artificiale — approvato il progetto per ricerca, imprese e pubblica amministrazione

Triennale Milano — gli eventi dal 3 all’8 marzo 2026 tra spettacoli, incontri e musica dal vivo

Roma — Malattie rare, ASL Roma 1 presenta il nuovo portale e iniziative di prossimità per i pazienti
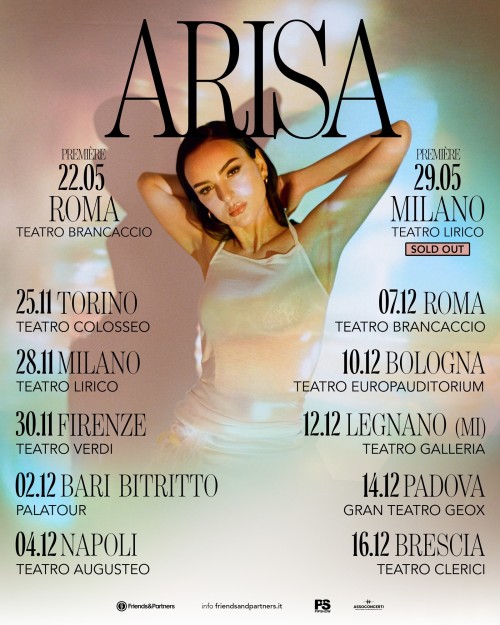
Sanremo — Arisa in gara con Magica Favola, sold out a Milano e tour nei teatri da novembre

Fender personalizzati ad alte prestazioni — la nuova protezione smart e sostenibile per barche e navi

Milano: a marzo partono i lavori in via Bramante, Torino e Cesare Correnti — riqualificazione strade e binari

Arisa: Magica Favola — tra le prime cinque a Sanremo — online il video e live a Roma e Milano

Levante: esce “Sei tu” dopo l’Ariston — nuovo singolo e tour 2026 nei club italiani

UN LETTO PER DUE: 35 ANNI D’AMORE TRA PASSIONE, TRADIMENTI E RIMPIANTI AL TEATRO SAN BABILA DI MILANO